Introduction
Dog bites pose a significant public health issue worldwide. According to the World Health Organization (WHO), dog bites account for tens of millions of injuries annually across the globe (https://www.who.int/news-room/fact-sheets/detail/rabies). Dog bites can lead to physical trauma as well as psychological distress. In severe cases, dog bites can cause infections or even rabies if the biting dog is infected.
To address this major concern, the WHO has published recommendations and protocols for the management of dog bites. This comprehensive guide covers critical information for healthcare providers, victims, families and communities. Key topics include severity assessment, first aid, medical treatment, emotional support, reporting procedures and prevention strategies.
This article provides an overview of the WHO’s authoritative recommendations for dog bite management. Major sections will cover bite severity, first aid, medical treatment, emotional support, reporting, and prevention measures. The goal is to summarize the WHO protocols into an accessible guide for anyone dealing with this unfortunate yet widespread issue.
Scope of the Problem

Dog bites pose a considerable public health issue worldwide. According to the U.S. Centers for Disease Control and Prevention (CDC), dogs bite over 4.5 million people each year in the United States alone, resulting in tens of thousands of reconstructive surgeries and hospitalizations [1]. Globally, the WHO estimates tens of millions of people suffer dog bites annually. Children are the most common victims, with over 50% of dog bites among children ages 5-9. Dog bites are also one of the leading causes of non-fatal injuries globally [2].
In addition to physical trauma, dog bites can lead to emotional distress, anxiety, and post-traumatic stress. Dog bites often require expensive medical treatment, reconstructive surgery, hospitalization, and rehabilitation. The CDC estimates over $1 billion is spent annually on dog bite-related hospitalizations in the U.S. alone [1]. Globally, dog bites have considerable economic impacts on individuals, families, communities, and health systems.
Certain populations are at higher risk of dog bites including children, the elderly, those with mental disabilities, mail carriers, and utility workers. Children are often unable to recognize warning signs from dogs and their short stature means they are more likely to be bitten on the head, face and neck. The elderly may have slower reflexes and weaker defenses to fend off an attack. Individuals with mental disabilities may also have difficulty reading a dog’s body language.
Causes and Risk Factors
Dogs bite for a variety of reasons. Some key causes and risk factors for dog bites include:
Lack of training and socialization – Dogs that are not properly socialized from a young age are more likely to be fearful or aggressive towards people and other animals. Poor supervision and neglect can also lead to problematic behaviors (Source).
Territorial behavior – Some dogs are more protective of their territory and may bite out of fear or a desire to guard. This is especially true for intact male dogs (Source).
Protecting resources – Dogs may bite to guard food, toys, or other possessions. Children getting too close to a dog’s food or trying to take away a toy are common scenarios.
Provocation – Dogs may bite after being teased, hit, cornered, or hurt. Even normally friendly dogs can bite if provoked.
Pain or illness – Dogs in pain or with underlying medical issues may bite more readily.
While some breeds like pit bulls or Rottweilers are often implicated in severe bites, most experts agree that situational factors are more predictive of biting than breed alone. Ultimately any dog is capable of biting given the right circumstances (Source).
Bite Severity
There are several classification systems used to assess the severity of dog bites. One commonly used scale was developed by Dr. Ian Dunbar, which categorizes bites into six levels:

Level 1 – Dog snaps or air bites without making contact. This demonstrates poor bite inhibition but no damage is done.
Level 2 – Dog makes skin contact but does not puncture the skin. May leave a bruise or minor surface abrasion.
Level 3 – Punctures the skin with a single tooth, but does not tear tissue. Minor punctures leave clear imprints of teeth.
Level 4 – One to four punctures from a single bite deeper than half the length of the dog’s canine teeth. Deeper punctures with redness and bruising. Tears tissue and muscle contractions are possible.
Level 5 – Multiple-bite incident with at least two Level 4 bites. Potential for substantial tissue and muscle damage. Bones may be exposed.
Level 6 – Attack resulting in death of a human. [1]
Assessing the potential damage and severity level of a dog bite helps determine the urgency of medical treatment needed. Levels 1 and 2 may be treated at home with first aid. Levels 3 and above require medical attention, with higher severity levels needing immediate emergency care to assess and treat potential muscle or nerve damage.
[1] Dr. Ian Dunbar’s Dog Bite Scale (Official Authorized Version)
First Aid
Stopping any bleeding is the first priority after a dog bite. Apply firm, direct pressure to the wound with a clean, dry cloth to help stop bleeding. Once bleeding subsides, gently wash the wound with soap and water, and rinse away any dirt or debris. Be sure to clean the wound thoroughly to help prevent infection, but do not scrub or irritate the wound. Pat dry with a clean towel.
After cleaning, apply an antibiotic ointment to help prevent infection. Cover the wound with a sterile bandage or clean cloth. Wrap the wound loosely to avoid cutting off blood flow. Check the bandage periodically and change if it becomes wet or dirty. Keeping the wound clean and covered helps prevent infection. According to Mount Sinai, signs of infection include increased pain, swelling, redness around the wound, red streaks, pus, or fever.
For minor bites, you may be able to tend to the wound yourself using proper first aid. But for deep wounds, extensive bleeding, or bites to the face, hands, or genitals, it’s important to seek medical care promptly. The risk of dangerous infection is higher with severe or complex wounds. Medical professionals can provide a thorough cleaning and examination, determine if stitches are needed, and prescribe antibiotics if necessary.
Sources:
https://www.mountsinai.org/health-library/selfcare-instructions/animal-bites-self-care
Medical Treatment
Seeing a doctor is recommended for all but the most minor dog bites that don’t break the skin. Deeper puncture wounds and bites to the face, hands, or genitals warrant immediate medical attention due to the risk of infection or damage to underlying structures like tendons, nerves or blood vessels.
Doctors will carefully clean the wound then determine if antibiotics are necessary. Dog bites have a high risk of infection so antibiotics may be prescribed even if there are no immediate signs of infection. Common antibiotics used include amoxicillin-clavulanate (Augmentin), doxycycline, and penicillin VK. The typical course is 3-5 days for minor bites and 7-10 days for more severe injuries.
Sutures or surgery may be required for larger wounds, especially if there is significant tissue damage. This helps properly align the tissue layers and minimize scarring. Plastic surgery may later be done for some facial injuries. Nerve or tendon damage also requires surgical repair.
Tetanus immunization should be updated if needed as dog bites pose a risk of tetanus infection. Rabies shots are given if the dog’s vaccine status is unknown. Imaging tests like x-rays or CT scans check for any underlying bone fractures or joint injuries.
Emotional Support
Being attacked by a dog can lead to significant anxiety, fear, or trauma, especially in children. This is true even if the dog is an emotional support animal that is normally well-behaved. According to the law firm Penney Lawyers, “The psychological impacts from an ESA attack can manifest immediately following the attack or even months later as the victim continues to deal with the trauma”(source). Seeking counseling and emotional support is important for recovering from the psychological impacts.
Options for emotional support include:
- Talking to friends and family for comfort
- Seeking counseling from a therapist or psychologist that specializes in trauma and dog bites
- Joining a support group with others who have experienced dog attacks
- Working with a counselor to overcome trauma, fear, and anxiety related to dogs
The emotional impacts of a dog attack should not be underestimated. Taking steps to process the trauma, get support, and recover emotionally is an important part of healing after an incident.
Reporting
If you or someone you know has been bitten by a dog, it’s important to report the incident to local authorities. Here are some key things to know about reporting dog bites:
You should contact animal control or law enforcement as soon as possible after the bite occurs. Many jurisdictions require dog bites to be reported within 24 hours.[1]
When you file the report, provide as many details as possible about the dog and its owner, including name, address, and description of the dog. The report should include where and when the bite happened. Having this information will help authorities locate the dog and follow up as needed.
After filing the initial report, follow up with animal control or the investigating agency periodically for updates. You may need to provide additional statements. Make sure to comply with requests to facilitate the investigation.
The report provides important legal documentation if you decide to pursue any action against the dog’s owner. It also helps authorities track bite incidents and dangerous dogs in the community.
Prevention
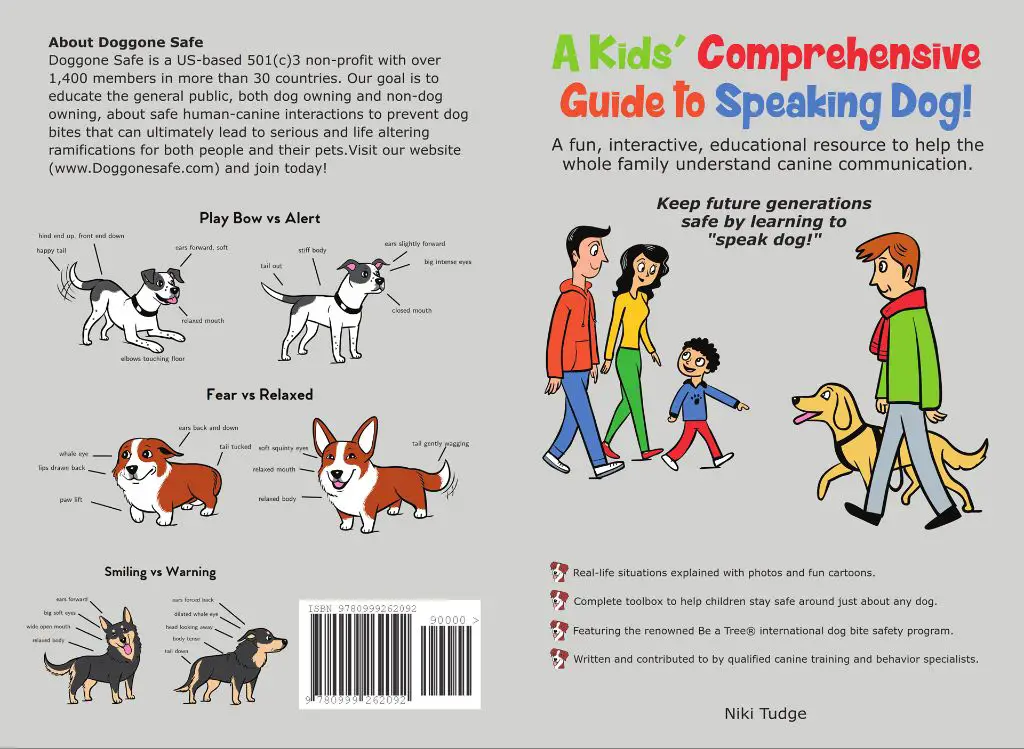
There are several strategies that can help prevent dog bites and reduce risk, including education, awareness, and policy considerations. According to the ASPCA, dog bite prevention should focus on teaching both children and adults how to interact safely around dogs. This includes never approaching an unfamiliar dog without permission, avoiding direct eye contact, and refraining from touching or petting a dog unless it initiates or the owner gives permission (1).
The CDC recommends teaching children basic safety around dogs, such as not disturbing a dog that is sleeping or eating, leaving dogs alone when they are caring for puppies, and not petting dogs through fences (2). Supervising young children around any dog is also critically important. For adults, prevention involves understanding dog body language and warning signs like growling or baring teeth. Adults should also avoid overly excitable play with dogs.
From a policy perspective, dangerous dog laws, leash laws, spay/neuter programs, and educational programs for owners about safety and training can help reduce dog bites. Some communities have enacted breed-specific legislation targeting breeds like pit bulls, but the CDC has found such policies controversial and ineffective (2). More holistic and comprehensive policy approaches seem to yield better prevention results.
(1) https://www.aspca.org/pet-care/dog-care/dog-bite-prevention
(2) https://www.cdc.gov/homeandrecreationalsafety/dog-bites/prevention.html
Conclusions
Following the proper protocol for dog bite management is crucial for preventing rabies infection and further complications. This article has covered the key steps that should be taken, including:
- Immediately washing the wound for at least 15 minutes and applying disinfectant
- Getting medical attention to assess bite severity and determine if stitches or antibiotics are needed
- Beginning post-exposure prophylaxis (PEP) rabies treatment if warranted based on bite location, wound severity, and local rabies risk
- Reporting the bite to authorities to facilitate rabies monitoring/testing of the animal if possible
- Providing emotional support for bite victims who may be traumatized
- Educating families, especially children, on safe behavior around dogs to prevent bites
While most dog bites are not life-threatening with proper care, rabies can have severe consequences if left untreated. Following WHO and CDC guidelines for dog bite management is the best way to avoid rabies infection and ensure bite wounds heal properly. This protocol should be understood by all healthcare workers and pet owners to prevent rabies transmission and bite-related complications.